170 Urine
Physical Characteristics of Urine
Urine is a sterile waste product composed of water soluble nitrogen products.
Learning Objectives
List the physical characteristics of urine
Key Takeaways
Key Points
- Urine color is an indicator for hydration.
- Urine pH is often influenced by diet.
- Urine smell indicates age of the urine and may indicate the prescence of glucose and ketones.
- Urine turbidity may indicate urinary tract infection or obstruction.
- Urinalysis is the process of analyzing and detecting chemicals excreted in urine.
- Physical characteristics of urine include color, smell, pH, density and turbidity
Key Terms
- urine: A liquid excrement consisting of water, salts, and urea, which is made in the kidneys then released through the urethra.
- urinalysis: A urinalysis (UA), also known as Routine and Microscopy (R&M), is an array of tests performed on urine, and one of the most common methods of medical diagnosis.
Urine, a typically sterile liquid by-product of the body, is secreted by the kidneys through a process called urination and excreted through the urethra. Urine is often used as a diagnostic feature for many disease conditions. These may b based on either physical or chemical components, that may give insight to processes within the body, often through urinalysis, a common clinical analysis of urine.
Physical Characteristics
Physical characteristics that can be applied to urine include color, turbidity (transparency), smell (odor), pH (acidity – alkalinity) and density. Many of these characteristics are notable and identifiable by by vision alone, but some require laboratory testing.
- Color: Typically yellow-amber, but varies according to recent diet and the concentration of the urine. Drinking more water generally tends to reduce the concentration of urine, and therefore causes it to have a lighter color. Dark urine may indicate dehydration. Red urine indicates red blood cells within the urine, a sign of kidney damage and disease.
- Smell: The smell of urine may provide health information. For example, urine of diabetics may have a sweet or fruity odor due to the presence of ketones (organic molecules of a particular structure) or glucose. Generally fresh urine has a mild smell but aged urine has a stronger odor similar to that of ammonia.
- The pH of normal urine is generally in the range 4.6 – 8, with a typical average being around 6.0. Much of the variation occurs due to diet. For example, high protein diets result in more acidic urine, but vegetarian diets generally result in more alkaline urine (both within the typical range of 4.6 – 8).
- Density: Density is also known as “specific gravity.” This is the ratio of the weight of a volume of a substance compared with the weight of the same volume of distilled water. The density of normal urine ranges from 0.001 to 0.035.
- Turbidity: The turbidity of the urine sample is gauged subjectively and reported as clear, slightly cloudy, cloudy, opaque or flocculent. Normally, fresh urine is either clear or very slightly cloudy. Excess turbidity results from the presence of suspended particles in the urine, the cause of which can usually be determined by the results of the microscopic urine sediment examination. Common causes of abnormal turbidity include: increased cells, urinary tract infections or obstructions.
Abnormalities in any of these of physical characteristics may indicate disease or metabolic imbalances. These problems may seem superficial or minor on their own, but can actually be the symptoms for more serious diseases, such as diabetes mellitus, or a damaged glomerulus.
Chemical Composition of Urine
Normal urine consists of water, urea, salts, and pigments.
Learning Objectives
Describe how normal urine consists of water, urea, salts and pigment
Key Takeaways
Key Points
- Urine is a liquid by-product of the body secreted by the kidneys through a process called urination and excreted through the urethra.
- Urine is an aqueous solution of greater than 95% water. Other constituents include urea, chloride, sodium, potassium, creatinine and other dissolved ions, and inorganic and organic compounds.
- Urea is a non-toxic molecule made of toxic ammonia and carbon dioxide. Any abnormal constituents found in urine are an indication of disease.
- The presence of red blood cells in urine is referred to as haematuria.
- The presence of proteins, which are normally too large to pass through the tubules, can be an indication of damage to the tubules, and is called proteinuria.
Key Terms
- urine: A liquid excrement that consists of water, salts, and urea, and is made in the kidneys then released through the urethra.
- diabetes: A group of endocrine diseases whereby a person has high blood sugar due to an inability to produce, metabolize, or respond to the hormone insulin.
Urine is a liquid byproduct of the body secreted by the kidneys through a process called urination and excreted through the urethra. The normal chemical composition of urine is mainly water content, but it also includes nitrogenous molecules, such as urea, as well as creatinine and other metabolic waste components.
Other substances may be excreted in urine due to injury or infection of the glomeruli of the kidneys, which can alter the ability of the nephron to reabsorb or filter the different components of blood plasma.
Normal Chemical Composition of Urine
Urine is an aqueous solution of greater than 95% water, with a minimum of these remaining constituents, in order of decreasing concentration:
- Urea 9.3 g/L.
- Chloride 1.87 g/L.
- Sodium 1.17 g/L.
- Potassium 0.750 g/L.
- Creatinine 0.670 g/L.
- Other dissolved ions, inorganic and organic compounds (proteins, hormones, metabolites).
Urine is sterile until it reaches the urethra, where epithelial cells lining the urethra are colonized by facultatively anaerobic gram-negative rods and cocci. Urea is essentially a processed form of ammonia that is non-toxic to mammals, unlike ammonia, which can be highly toxic. It is processed from ammonia and carbon dioxide in the liver.
Abnormal Types of Urine
There are several conditions that can cause abnormal components to be excreted in urine or present as abnormal characteristics of urine. They are mostly referred to by the suffix -uria. Some of the more common types of abnormal urine include:
- Proteinuria—Protein content in urine, often due to leaky or damaged glomeruli.
- Oliguria—An abnormally small amount of urine, often due to shock or kidney damage.
- Polyuria—An abnormally large amount of urine, often caused by diabetes.
- Dysuria—Painful or uncomfortable urination, often from urinary tract infections.
- Hematuria—Red blood cells in urine, from infection or injury.
- Glycosuria— Glucose in urine, due to excess plasma glucose in diabetes, beyond the amount able to be reabsorbed in the proximal convoluted tubule.
Regulation of Urine Concentration and Volume
Antidiuretic hormone (ADH) is produced by the pituitary gland to control the amount of water that is reabsorbed through the collecting ducts.
Learning Objectives
Describe how regulating the amount of water excreted in urine is an essential component of homeostasis that is regulated by the antidiuretic hormone (ADH)
Key Takeaways
Key Points
- Urine volume and concentration is regulated through the same processes that regulate blood volume.
- Antidiuretic hormone (ADH)—produced by the posterior pituitary gland —increases the amount of water reabsorbed in the distal convoluted tubule and collecting duct.
- Osmoreceptors in the hypothalamus signal the posterior pituitary gland to increase ADH secretion when plasma osmolarity becomes too high.
- ADH causes decreased urine volume and decreased plasma osmolarity.
- A diuretic increases urine volume and increases plasma osmolarity.
- Common diuretics include alcohol, water, caffeine, and many medications, and they generally function as diuretics via different mechanisms.
Key Terms
- diuretic: A substance that increases urine volume and increases plasma osmolarity, often by inhibiting ADH secretion to prevent water reabsorption in the nephron.
- antidiuretic hormone: A hormone secreted by the posterior pituitary gland that increases water retention to decrease urine volume and decrease plasma osmolarity.
Urine is produced not only to eliminate many cellular waste products, but also to control the amount of water in the body. In a way, urine volume regulation is part of homeostasis, in that it directly regulates blood volume, because greater amounts of urine will reduce the volume of waters in blood.
There are a few complex systems involved in regulating blood volume and urine production, such as the intricate renin–angiotensin system, and the simpler anti-diuretic hormone (ADH) feedback system.
Anti-Diuretic Hormone Feedback
An anti-diruetic is a substance that decreases urine volume, and ADH is the primary example of it within the body. ADH is a hormone secreted from the posterior pituitary gland in response to increased plasma osmolarity (i.e., increased ion concentration in the blood), which is generally due to an increased concentration of ions relative to the volume of plasma, or decreased plasma volume.
The increased plasma osmolarity is sensed by osmoreceptors in the hypothalamus, which will stimulate the posterior pituitary gland to release ADH. ADH will then act on the nephrons of the kidneys to cause a decrease in plasma osmolarity and an increase in urine osmolarity.
ADH increases the permeability to water of the distal convoluted tubule and collecting duct, which are normally impermeable to water. This effect causes increased water reabsorption and retention and decreases the volume of urine produced relative to its ion content.
After ADH acts on the nephron to decrease plasma osmolarity (and leads to increased blood volume) and increase urine osmolarity, the osmoreceptors in the hypothalamus will inactivate, and ADH secretion will end. Due to this response, ADH secretion is considered to be a form of negative feedback.
Diuretics
A diuretic is any substance that has the opposite effect of ADH— they increase urine volume, decrease urine osmolarity, lead to an increased plasma osmolarity, and often reduced blood volume. Many substances can act as diuretics, albeit with different mechanisms.
A common example is alcohol and water ingestion, which directly inhibit ADH secretion in the pituitary gland. Alternatively caffeine is a diuretic because it interferes with sodium reabsorption (reducing the amount of water reabsorbed by sodium cotransport) and increases the glomerular filtration rate by temporarily increasing blood pressure. Many medications are diuretics because they inhibit the ATPase pumps, thus slowing water reabsorption further.
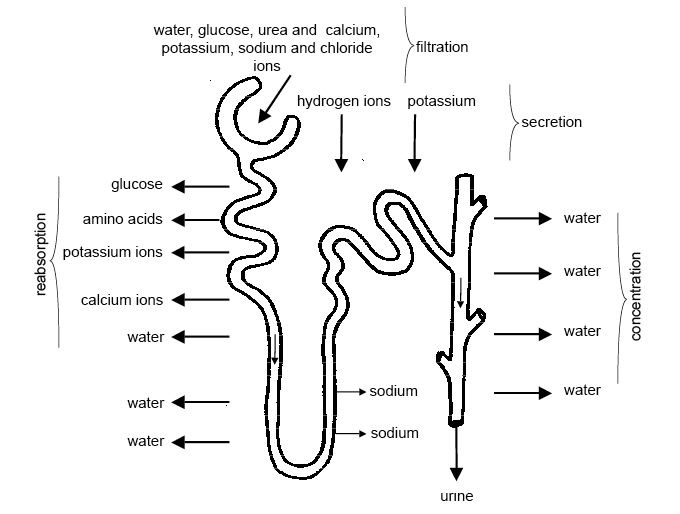
Summary of the process of urine formation: As the fluid flows along the proximal convoluted tubule useful substances like glucose, water, salts, potassium ions, calcium ions, and amino acids are reabsorbed into the blood capillaries that form a network around the tubules. Many of these substances are transported by active transport and energy is required.
Urinalysis
Urinalysis is the process of analyzing urine for target parameters of health and disease.
Learning Objectives
Describe how urinalysis can be used as a method of diagnosis in medicine
Key Takeaways
Key Points
- The characteristics that can be detected in urine include cells, substances, and properties, such as specific gravity or pH.
- Urinalysis can be performed on test strips (routine) by light microscopy.
- The numbers and types of cells and/or material, such as urinary casts, can yield a great detail of information and may suggest a specific diagnosis.
- Urinary casts include hyaline casts, granular casts, white blood cell casts, red blood cell casts, epithelial cell casts, or bacterial cell casts, which all indicate different abnormalities within urine.
Key Terms
- urinary cast: Tiny structures formed from bound abnormal cells and molecules within the nephrons that are excreted in urine.
- urinalysis: Also known as routine and microscopy (R&M), this is an array of tests performed on urine, and one of the most common methods of medical diagnosis.
Urinalysis
A urinalysis (UA), also known as routine and microscopy (R&M), is an array of tests performed on urine, and one of the most common methods of medical diagnosis. Urinalysis means the analysis of urine, and it is used to diagnose several diseases.
The target parameters that are measured or quantified in urinalysis include many substances and cells, as well as other properties, such as specific gravity. A part of a urinalysis can be performed by using urine test strips, in which the test results can be read as the strip’s color changes. Another method is light microscopy of urine samples.
When doctors order a urinalysis, they will request either a routine urinalysis or a routine and microscopy (R&M) urinalysis; the difference being that a routine urinalysis does not include microscopy or culture. R&M is used specifically for culturing bacteria found in urine, which can make it an important tool for diagnosing specific urinary tract infections.
Test Strip Urinalysis
Test strip urinalysis exposes urine to strips that react if the urine contains certain cells or molecules. Test strip urinalysis is the most common technique used in routine urinalysis. A urine test strip can identify:
- Leukocytes—their presence in urine is known as leukocyturia.
- Nitrites—their presence in urine is known as nitrituria.
- Proteins —their presence in urine is known as proteinuria, albuminuria, or microalbuminuria.
- Blood—its presence in urine is known as hematuria.
- pH—the acidity of urine is easily quantified by test strips, which can identify cases of metabolic acidosis or alkalosis.
Urine Microscopy
The numbers and types of cells and/or material, such as urinary casts, can yield a great detail of information and may suggest a specific diagnosis. A urinary cast is any tiny structure found in urine that consists of multiple molecules or cells bound together.
Casts form within the nephron when abnormal cells and molecules are filtered from blood, and are excreted as the bound structures in urine. Microscopy can identify casts in urine and use them to diagnose kidney diseases, by characterizing symptoms such as:
- Red blood cell casts are associated with glomerulonephritis, vasculitis, or malignant hypertension.
- White blood cell casts are associated with acute interstitial nephritis, exudative glomerulonephritis, or severe pyelonephritis.
- Epithelial cell casts are associated with toxin-induced, acute tubular necrosis, hepatitis, and cytomegalovirus.
- (Heme) granular casts are associated with acute tubular necrosis, and are often composed of proteins, especially antibodies.
- Hyaline casts are associated with dehydration; it is the most common type of cast.
- Bacterial casts are associated with urinary tract infection; the cast may be cultured in order to identify the causative organism of the cast.

Urinalysis: White blood cells seen under a microscope from a urine sample.
Renal Clearance
Clearance is a measurement of the renal excretion ability.
Learning Objectives
Describe how clearance is a measure of the renal excretion ability
Key Takeaways
Key Points
- Each substance has a specific clearance that depends on its filtration characteristics, size, and molecular structure.
- Clearance is dependent upon glomerular filtration, secretion, and reabsorption.
- Clearance may be either constant or variable over time.
- Many drugs can either be bound to plasma proteins or unbound in plasma; however, they will not be cleared from the body when bound to proteins.
- Renal clearance is the main form of clearance in the body, and when combined with other routes of clearance in the body it accounts for most of the total body clearance.
Key Terms
- nephron: The basic structural and functional unit of the kidney that filters the blood in order to regulate chemical concentrations and thereby produce urine.
- Renal clearance: The rate at which a substance is removed from the plasma via renal system activity over a unit of time.
Clearance
In renal physiology, clearance is a measurement of the renal excretion ability, which measures the amount of plasma from which a substance is removed from the body over an interval of time. Each substance has its own specific clearance that depends on its unique filtration characteristics.
Clearance is a function of glomerular filtration, secretion from the peritubular capillaries to the nephron, and reabsorption from the nephron back to the peritubular capillaries. Clearance can be either a constant or variable component over time, depending on the type of substance.

Physiology of the nephron: Diagram showing the basic physiologic mechanisms of the kidney.
Clearance Mechanisms
Renal clearance depends mainly on GFR, tubular absorption, and tubular secretion. If any of those variables change, the renal clearance rate of a substance will change as well. These variables alter clearance through the following rules:
- Increased GFR will increase clearance, while decreased GFR will decrease clearance.
- Increased tubular secretion will increase clearance, while decreased tubular secretion will decrease clearance. This variable is sometimes altered through changes in the expression of ATPase pumps involved in active transport.
- Increased tubular reabsorption will decrease clearance, while increased tubular reabsorption will increase clearance.
Additionally, the characteristics of the substance of interest will also determine some components of clearance. For example, certain pharmaceuticals have the tendency to bind to plasma proteins or exist unbound in plasma. Only those that are unbound will be filtered and cleared from the body. Size and molecular structure will also alter the clearance rate.
It is also important to note that renal clearance is not the only form of clearance that occurs for the substances within the plasma of the body. The other types of clearance are
- Biliary (through bile).
- Salivary.
- Pulmonary clearance (removed during alveolar gas exchange).
These types of clearance may also excrete certain molecules from the bloodstream based on their size and molecular structure; however, these forms of clearance are generally relatively minor compared to renal clearance.
These types of clearance all add up to a summation known as total body clearance, which refers to the removal of a substance from the plasma over time, incorporating all routes of removal in the body.
