88 Hormones
Mechanisms of Hormone Action
A hormone is a secreted chemical messenger that enables communication between cells and tissues throughout the body.
Learning Objectives
Summarize the mechanisms of hormone action
Key Takeaways
Key Points
- Hormones are released into the bloodstream through which they travel to target sites.
- The target cell has receptors specific to a given hormone and will be activated by either a lipid-soluble (permeable to plasma membrane) or water-soluble hormone (binds to a cell-surface receptor).
- Lipid-soluble hormones diffuse through the plasma membrane to enter the target cell and bind to a receptor protein.
- Water-soluble hormones bind to a receptor protein on the plasma membrane of the cell.
- Receptor stimulation results in a change in cell activity, which may send feedback to the original hormone-producing cell.
Key Terms
- Water-soluble hormone: A lipophobic hormone that binds to a receptor on, or within, the plasma membrane, to initiate an intracellular signaling cascade.
- hormone: A molecule released by a cell or a gland in one part of the body that sends out messages affecting cells in other parts of the organism.
- Lipid-soluble hormone: A lipophilic hormone that passes through the plasma membrane of a cell, binds to an intracellular receptor, and changes gene expression.
A hormone is a chemical messenger that enables communication between cells. Hormones are secreted by the glands of the endocrine system and they serve to maintain homeostasis and to regulate numerous other systems and processes, including reproduction and development.
Hormone Signaling
The glands of the endocrine system secrete hormones directly into the extracellular environment. The hormones then diffuse to the bloodstream via capillaries and are transported to the target cells through the circulatory system. This allows hormones to affect tissues and organs far from the site of production or to apply systemic effects to the whole body.
Hormone-producing cells are typically specialized and reside within a particular endocrine gland, such as thryocytes in the thyroid gland. Hormones exit their cell of origin through the process of exocytosis or by other means of membrane transport.
Cellular recipients of a particular hormonal signal may be one of several cell types that reside within a number of different tissues. This is so in the case of insulin, which triggers a diverse range of systemic physiological effects. Different tissue types may also respond differently to the same hormonal signal. As a result, hormonal signaling is elaborate and hard to dissect.
Hormones activate target cells by diffusing through the plasma membrane of the target cells (lipid-soluble hormones) to bind a receptor protein within the cytoplasm of the cell, or by binding a specific receptor protein in the cell membrane of the target cell (water-soluble proteins). In both cases, the hormone complex will activate a chain of molecular events within the cell that will result in the activation of gene expression in the nucleus.
The reaction of the target cells may then be recognized by the original hormone-producing cells, leading to a down-regulation in hormone production. This is an example of a homeostatic negative feedback loop.

Lipid-soluble hormone receptor activation: Nuclear hormone receptors are activated by a lipid-soluble hormone such as estrogen, binding to them inside the cell. Lipid-soluble hormones can cross the plasma membrane.
Steps of Hormonal Signaling
- Biosynthesis of a particular hormone in a particular tissue.
- Storage and secretion of the hormone.
- Transport of the hormone to the target cells, tissues, or organs.
- Recognition of the hormone by an associated cell membrane or an intracellular receptor protein.
- Relay and amplification of the received hormonal signal via a signal transduction process.
- Potential feedback to a hormone-producing cell.
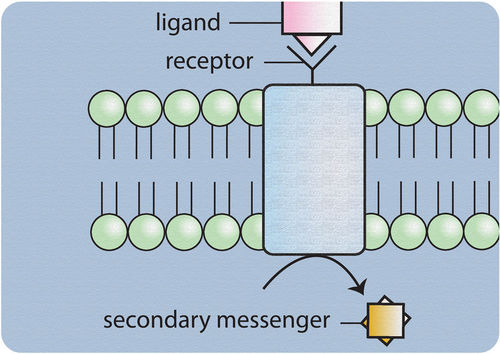
Water-soluble hormone receptor activation: Water-soluble hormones, such as epinephrine, bind to a cell-surface localized receptor, initiating a signaling cascade using intracellular second messengers.
Hormone Classes
Hormones are typically divided into three classes:
- Peptide: Hormones that are modified amino acids or short (peptide) or long (protein) chains of amino acids. Additionally, they can contain carbohydrate moieties.
- Lipid: Steroid hormones that contain lipids synthesized from cholesterol and eicosanoids that contain lipids synthesized from the fatty acid chains of phospholipids found in the plasma membrane.
- Monoamine: Hormones derived from aromatic amino acids such as
phenylalanine, tyrosine, and tryptophan.
Hormone Receptors
Hormones activate a cellular response in the target cell by binding to a specific receptor in the target cell.
Learning Objectives
Distinguish between the location and function of hydrophilic and lipophilic hormone receptors
Key Takeaways
Key Points
- For water-soluble proteins, the receptor will be at the plasma membrane of the cell.
- The ligand-bound receptor will trigger a cascade of secondary messengers inside the cell.
- For lipid-soluble hormones, the receptor is typically located within the cytoplasm or nucleus of the cell.
- The binding of the hormone allows the receptor to influence transcription in the nucleus, either alone or in association with other transcription factors.
- The number of hormone molecules is usually the key factor for determining hormone action and it is determined by the concentration of circulating hormones, which in turn is influenced by the rate and level of secretion.
- Another limiting factor for hormone action is the effective concentration of hormone-bound receptor complexes that are formed within the cell. This is determined by the number of hormone/receptor molecules available for complex formation and the binding affinity between the hormone and receptor.
Key Terms
- secondary messenger: These are molecules that relay signals from receptors on the cell surface to target molecules inside the cell, in the cytoplasm, or the nucleus.
A hormone receptor is a molecule that binds to a specific hormone. Receptors for peptide hormones tend to be found on the plasma membrane of cells, whereas receptors for lipid-soluble hormones are usually found within the cytoplasm.
Upon hormone binding, the receptor can initiate multiple signaling pathways that ultimately lead to changes in the behavior of the target cells.
The hormone activity within a target cell is dependent on the effective concentration of hormone-receptor complexes that are formed. The number of these complexes is in turn regulated by the number of hormone or receptor molecules available, and the binding affinity between hormone and receptor.
Lipophobic Hormones
Many hormones are composed of polypeptides—such as thyroid -stimulating hormones, follicle-stimulating hormones, luteinizing hormones, and insulin. These molecules are not lipid-soluble and therefore cannot diffuse through cell membranes.
The receptors for these hormones need to be localized to the cells’ plasma membranes. Following an interaction with the hormones, a cascade of secondary effects within the cytoplasm of the cell is triggered, often involving the addition or removal of phosphate groups to cytoplasmic proteins, changes in ion channel permeability, or an increase in the concentrations of intracellular molecules that may act as secondary messengers, such as cyclic AMP.
Lipophilic Hormones
Lipophilic hormones—such as steroid or thyroid hormones—are able to pass through the cell and nuclear membrane; therefore receptors for these hormones do not need to be, although they sometimes are, located in the cell membrane.
The majority of lipophilic hormone receptors are transcription factors that are either located in the cytosol and move to the cell nucleus upon activation, or remain in the nucleus waiting for the steroid hormone to enter and activate them.
Upon binding by the hormone the receptor undergoes a conformational change, and the receptor together with the bound hormone influence transcription, either alone or in association with other transcription factors.

Example hormone receptor: The thyroid hormone receptor (TR) heterodimerized to the RXR. In the absence of a ligand, the TR is bound to a corepressor protein. Ligand binding to the TR causes a dissociation of co-repressor and recruitment of co-activator proteins, which in turn recruit additional proteins (such as RNA polymerase) that are responsible for the transcription of downstream DNA into RNA, and eventually into protein that results in a change in cell function.
Chemistry of Hormones
There are three classes of hormones: peptide hormones, lipid hormones, and monoamine hormones.
Learning Objectives
Distinguish between the hydrophilic and lipophilic types of endocrine hormones based on their chemical structures
Key Takeaways
Key Points
- Peptide hormones are comprised of short (peptides) and long ( proteins ) chains of amino acids. They are water-soluble but cannot pass through the plasma membrane alone.
- Glyco-protein hormones have a carbohydrate moiety attached to the protein.
- Lipid hormones include steroid and eicosanoid hormones. They are lipid-soluble and can pass through the plasma membrane.
- Steroid hormones are derived from the cholesterol and eicosanoid hormones from fatty acids that compose the plasma membrane.
- The third class of hormones is the monoamines that are derived from aromatic amino acids like phenylalanine, tyrosine, and tryptophan.
A hormone is a chemical released by a cell or a gland in one part of the body that sends out messages that affect cells in other parts of the organism.
There are three classes of hormones:
- Peptide hormones
- Lipid-derived hormones
- Monoamine hormones
Peptide Hormones
Peptide hormones consist of short chains of amino acids, such as vasopressin, that are secreted by the pituitary gland and regulate osmotic balance; or long chains, such as insulin, that are secreted by the pancreas, which regulates glucose metabolism.
Some peptide hormones contain carbohydrate side chains and are termed glyco-proteins, such as the follicle-stimulating hormone. All peptide hormones are hydrophilic and are therefore unable to cross the plasma membrane alone.

Peptide hormone: Representation of the molecular structure of a peptide hormone.
Lipid-Derived Hormones
Lipid and phospholipid-derived hormones are produced from lipids such as linoleic acid and arachidonic acid. Steroid hormones, which form the majority of lipid hormones, are derived from carbohydrates; for example, testosterone is produced primarily in the testes and plays a key role in development of the male reproductive system.
Eicosanoids are also lipid hormones that are derived from fatty acids in the plasma membrane. Unlike other hormones, eicosanoids are not stored in the cell—they are synthesized as required. Both are lipophillic and can cross the plasma membrane.
Monoamine Hormones
Monoamine hormones are derived from single aromatic amino acids like phenylalanine, tyrosine, and tryptophan. For example, the tryptophan-derived melatonin that is secreted by the pineal gland regulates sleep patterns.
Transport of Hormones
Hormones synthesized by the endocrine glands are transported throughout the body by the bloodstream.
Learning Objectives
Describe the way in which hormones are transported in the endocrine system
Key Takeaways
Key Points
- Hormones are typically secreted into systemic circulation. However, some are secreted into portal systems that allow for direct hormone targeting.
- Hormones can exist freely in systemic circulation, but the majority are bound with transport proteins.
- Transport proteins hold hormones inactive in systemic circulation and create a reservoir within the circulation that facilitates an even distribution of hormones throughout the tissue or organ.
Key Terms
- transport protein: A protein that binds with a hormone in systemic circulation that facilitates its efficient transport.
The endocrine system is a system of ductless glands that secrete hormones directly into the circulatory system to be carried long distances to other target organs that regulate key body and organ functions.
Some endocrine glands secrete into a portal system rather than the systemic circulation that allows for the direct targeting of hormones. For example, hormones secreted by the pancreas pass into the hepatic portal vein that transports them directly to the liver.
Once within the circulatory system a small proportion of hormones circulate freely, however the majority are bound with a transport protein. Mainly produced in the liver, these transport proteins are hormone specific, such as the sex hormone binding globulin that binds with the sex hormones.
When bound with a transport protein hormones are typically inactive, and their release is often triggered in regions of low hormone concentration or can be controlled by other factors. Therefore, transport proteins can act as a reservoir within the circulatory system and help insure an even distribution of hormones within an organ or tissue.

The endocrine system: The major endocrine glands for men and women (male left, female on the right): 1. Pineal gland 2. Pituitary gland 3. Thyroid gland 4. Thymus 5. Adrenal gland 6. Pancreas 7. Ovary 8. Testis
