100 Overview of Blood
Components of Blood
Blood is composed of plasma and three types of cells: red blood cells, white blood cells, and platelets.
Learning Objectives
Differentiate among the blood components of erythrocytes, leukocytes, and thrombocytes
Key Takeaways
Key Points
- Red blood cells’ primary function is to transport oxygen between the lungs and tissues of the body.
- White blood cells, the cells of the immune system, provide defense against pathogens.
- Platelets are involved in clot formation during wound healing.
- Blood is an extracellular matrix tissue in which various blood cells are suspended in the plasma matrix.
- Blood is vital for normal metabolic function due to the transfer of oxygen, carbon dioxide, and glucose to and from the body’s tissues. It also transports a number of other cells and molecules throughout the body.
Key Terms
- plasma: The straw-colored or pale yellow liquid component of blood in which blood cells are suspended.
- hemoglobin: The iron-containing substance in red blood cells that binds to and transports oxygen from the alveoli of the lungs to the tissues of the body. It consists of a protein (globulin) and haem (a porphyrin ring with an atom of iron at its center).

Composition of Blood: Two tubes of EDTA-anticoagulated blood. Left tube: after standing, the RBCs have settled at the bottom of the tube.
Blood is a circulating tissue composed of fluid, plasma, and cells. The cellular components of blood are erythrocytes (red blood cells, or RBCs), leukocytes (white blood cells, or WBCs), and thrombocytes (platelets). By volume, the RBCs constitute about 45% of whole blood, the plasma about 54.3%, and white blood cells about 0.7%. Platelets make up less than 1%. Although it consists of cells suspended in fluid, blood is still considered a tissue as it is technically a type of extracellular matrix.
Blood enables transport of cells and molecules between parts of the body. Oxygen, carbon dioxide, and glucose are among the most vital molecules transported in blood. Blood cells are essential for normal metabolic and immune system function.
Erythrocytes (RBCs)
Erythrocytes are discs measuring about seven to eight micrometers in diameter. RBCs contain hemoglobin molecules which bind to oxygen so it can be transported to tissues. Mature RBCs lack a nucleus and organelles and have no nuclear DNA. RBCs, endothelial vessel cells, and other blood cells are also marked by glycoproteins that define the different blood types. The ratio of RBCs to blood plasma is referred to as the hematocrit, and is normally about 45%. The combined surface area of all red blood cells of the human body would be roughly 2,000 times greater than the body’s exterior surface.
Leukocytes (WBCs)
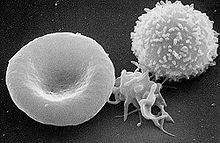
Components of Blood: From left to right, a diagram of an erythrocyte, thrombocyte, and leukocyte.
Leukocytes are usually larger in size (10–14 micrometers in diameter) than red blood cells. They lack hemoglobin but contain organelles, a nucleus, and nuclear DNA. WBCs are the main functional component of the body’s immune system. They destroy and remove old or aberrant cells and cellular debris, as well as attack infectious agents (pathogens) and foreign substances. There are several different types of white blood cells: basophils, eosinophils, neutrophils, monocytes, natural killer cells, B- and T-cell lymphocytes, macrophages, and dendritic cells, all of which perform distinct functions.
Thrombocytes (Platelets)
Thrombocytes measure between one to two micrometers in diameter. These membrane-bound cell fragments lack nuclei and are responsible for blood clotting (coagulation). They result from fragmentation of large cells called megakaryocytes, which are derived from stem cells in the bone marrow. Platelets are produced at a rate of 200 billion per day, a process regulated by the hormone thrombopoietin. Platelets contain mitochondrial DNA, but not nuclear DNA.
The sticky surface of platelets allows them to accumulate at the site of broken blood vessels to form a clot, due in part to the release of clotting factors that occurs during endothelial injury to blood vessels. This process is called hemostatis. Platelets secrete factors that increase local platelet aggregation (e.g., thromboxane A), enhance vasoconstriction (e.g., serotonin), and promote blood coagulation (e.g., thromboplastin, fibrinogen). Platelets are critically important for wound healing, which can only occur once the clot forms and bleeding ceases completely.
Physical Characteristics and Volume
Blood contains plasma and blood cells, some of which have hemoglobin that makes blood red. The average blood volume in adult is five liters.
Learning Objectives
Describe the physical characteristics and volume of blood in adults
Key Takeaways
Key Points
- Blood accounts for 8% of human body weight. The average adult has a blood volume of roughly five liters (1.3 gal).
- By volume, red blood cells constitute about 45% of whole blood, plasma about 54.3%, and white blood cells about 0.7%. Platelets make up less than 1%. Blood also contains proteins such as albumins.
- Hemoglobin is the principal determinant of blood color in vertebrates. Each molecule has four heme groups, and their interaction with various molecules alters the exact color of blood.
- Veins appear to be blue because blue light penetrates the skin better than other forms of light. Deoxygenated blood is not blue.
- Blood volume is a regulated variable that is proportional to blood pressure and a component of homeostasis.
- Injury can cause blood loss. A healthy adult can lose almost 20% of blood volume (1 L) before the first symptom (restlessness) begins, and 40% of volume (2 L) before hypovolemic shock sets in.
Key Terms
- erythrocyte: An anucleate cell in the blood involved with the transport of oxygen. Also called a red blood cell because of the red coloring of hemoglobin.
- hemoglobin: The iron-containing substance in red blood cells that transports oxygen from the lungs to the rest of the body. It consists of a protein (globulin) and haem (a porphyrin ring with an atom of iron at its center).
- tissue perfusion: The amount of blood that can reach the tissues to supply them with oxygen and glucose.
Blood is a specialized bodily fluid in animals that delivers necessary substances, such as nutrients and oxygen, to the cells and transports metabolic waste products away from those same cells. Blood plays many roles in sustaining life and has physical characteristics that distinguish it from other body tissues.
Physical Characteristics
Blood is a fluid that is technically considered a connective tissue. It is an extracellular matrix in which blood cells are suspended in plasma. It normally has a pH of about 7.4 and is slightly denser and more viscous than water. Blood contains red blood cells (RBCs), white blood cells (WBCs), platelets, and other cell fragments, molecules, and debris. Albumin is the main protein found in plasma, and it functions to regulate the colloidal osmotic pressure of blood.
Blood appears red because of the high amount of hemoglobin, a molecule found on RBCs. Each hemoglobin molecule has four heme groups that interact with various molecules, which alters the exact color. In oxygenated blood found in arterial circulation, hemoglobin-bound oxygen creates a distinctive red color.
Deoxygenated blood is a darker shade of red. It is present in veins and can be seen during blood donation or lab tests. Carbon monoxide poisoning causes bright red blood due to the formation of carboxyhemoglobin. In cyanide poisoning, venous blood remains oxygenated, increasing the redness. Under normal conditions, blood can never truly be blue, although most visible veins appear blue because only blue light can can penetrate deeply enough to illuminate veins beneath the skin.
Blood Volume
Blood generally accounts for 8% of the human body weight. The average adult has a blood volume of roughly five liters (1.3 gal). By volume, red blood cells constitute about 45% of whole blood, plasma about 54.3%, and white cells about 0.7%, with platelets making up less than 1%.

Composition of blood: Two tubes of EDTA-anticoagulated blood. Left tube: After standing, the RBCs have settled at the bottom of the tube. Right tube: contains freshly drawn blood.
Blood volume is a regulated variable that is directly proportional to blood pressure through the output of the heart. In order to maintain homeostasis, blood volume and blood pressure must be high enough that blood can reach all of the body’s tissues, a process called tissue perfusion. Most tissues can survive without perfusion for a short amount of time, but the brain needs a continuous supply of oxygen and glucose to stay alive.
Many mechanisms exist to regulate blood volume and tissue perfusion, including renal water excretion in the kidney, the pumping activity of the heart, and the abilities of the arteries to constrict or dilate. When blood volume becomes too low, such as from an injury, dehydration, or internal bleeding, the body will enter into a state of hypovolemic shock, in which tissue perfusion decreases too much. A healthy adult can lose almost 20% of blood volume (1 L) before the first symptom, restlessness, begins, and 40% of volume (2 L) before hypovolemic shock sets in. Conversely, higher than normal blood volume may cause hypertension, heart failure, and aneurysms.
Functions of Blood
The main function of blood is to supply oxygen to tissues and remove carbon dioxide. Other functions include pH regulation and thermoregulation.
Learning Objectives
Describe the functions blood performs in the body
Key Takeaways
Key Points
- The main function of blood is to carry oxygen from lungs and deliver it to the body, where it is released and carbon dioxide is consumed.
- The tissues of the body cannot survive without blood perfusion. Without blood, tissues may undergo hypoxia, ischemia, or infarction depending on the severity of the deficiency.
- The blood is involved in the homeostasis of variables such as temperature, blood volume, blood pressure, blood pH, and blood glucose levels.
- Other important blood functions include carbon dioxide transport and hormone signaling.
- The blood is involved in immune system functions such as white blood cell activity and blood clotting.
Key Terms
- hypoxia: A condition in which tissues are deprived of an adequate supply of oxygen for metabolic purposes; anoxia.
- coagulation: The process by which blood forms solid clots.
Blood performs many functions critical for sustaining metabolic physiological processes in complex organisms. Blood is involved in everything from gas exchange to nutrient transport to immune system and homeostatic functions.
Oxygen and Glucose Transport
Blood’s primary function is to transport molecules around the body to support critical metabolic processes. All cells require oxygen and glucose to undergo cellular respiration. Tissues cannot survive very long without these two molecules. Disruption of this process is most dangerous to the brain, which can survive only about two minutes without oxygen and glucose. These terms are used to describe oxygen or blood deficiency to tissues in the body:
- Hypoxia: a state in which the tissues do not receive adequate oxygen supply, generally due to decreased tissue perfusion or decreased oxygen intake.
- Ischemia: a reversible condition in which a tissue does not receive adequate blood supply, usually from an obstructed or ruptured blood vessel.
- Infarction: a usually irreversible condition in which tissues die as a result of prolonged oxygen or blood supply.
Most tissues can survive in a hypoxic or ischemic state for a few hours before infarction sets in. Heart infarction, which often occurs during a heart attack, will cause infarction in other tissues as blood is no longer pumped.
In addition to oxygen and glucose, the blood transports several other important molecules. Carbon dioxide, which travels through the blood mostly as bicarbonate, is transported from tissues as a waste product of cellular respiration to the lungs during gas exchange. Many hormones (chemical messengers) also travel through the blood as a form of communication between interrelated organs, which are often involved in homeostatic control.
Immune System Functions
Cellular Components of Blood: From left, diagrams of an erythrocyte, thrombocyte, and leukocyte.
White blood cells and antibodies circulate through the blood and destroy any foreign invaders ( pathogens ) that they encounter. Inflammation occurs in blood vessels due to the release of inflammatory mediators in the blood. This causes vasodilation and redness as other white blood cells are drawn to the region through the bloodstream to destroy infectious pathogens. They may also find molecular markers of pathogens called antigens and take them to lymphatic organs to stimulate powerful adaptive immune system responses.
The blood also has the ability to undergo clotting in response to vascular injury such as bleeding. Normally a series of clotting and anti-clotting factors are kept in balance through the blood so that no clotting occurs, but when endothelial cells are injured, the clotting factors are increased and cause blood to clot. Circulating platelets in the blood arrive at the injury site and form a mesh and plug to coagulate the blood and stop the bleeding. Wound healing can only begin after this clotting response occurs.
Homeostatic Functions
Blood is involved in maintaining homeostasis through several ways. Temperature regulation occurs in part as a result of the dilation and constriction of vessels in the blood. Blood pH is a regulated variable of the respiratory system, because the pH of blood is directly proportional to the amount of carbon dioxide dissolved in blood. This makes blood pH an indicator of respiratory homeostasis. Blood glucose levels are regulated by insulin and glucagon secretion. Blood volume and blood pressure are directly proportional regulated variables that are tied to the activity of the heart and the fluid retention of the kidney. If any of these variables are too high or too low, severe problems can occur. For that reason, a number of complex negative feedback mechanisms exist to keep all variables within homeostatic range, despite influences from the internal and external environments.
Blood Plasma
Plasma comprises about 55% of total blood volume. It contains proteins and clotting factors, transports nutrients, and removes waste.
Learning Objectives
Describe the features of blood plasma
Key Takeaways
Key Points
- The majority of blood volume consists of plasma. This aqueous solution is 92% water. It also contains blood plasma proteins, including serum albumin, blood-clotting factors, and immunoglobulins.
- Plasma circulates respiratory gases, dissolved nutrients, and other materials. It also removes waste products.
- Globulins are a diverse group of proteins that primarily transport other substances and inhibit certain enzymes.
- Albumins maintain osmotic balance between the blood and tissue fluids through exertion of oncotic pressure.
- Fibrinogen is the main clotting protein found in plasma. It is responsible for stopping blood flow during wound healing.
Key Terms
- platelet: A small, colorless, disc-shaped particle found in the blood of mammals. It plays an important role in blood clot formation.
- immunoglobulin: Any of the glycoproteins in blood serum that respond to invasion by foreign antigens and that protect the host by removing pathogens; an antibody.
- albumins: A plasma protein that exerts a high degree of oncotic pressure to pull water and other substances into tissues.
About 55% of blood is blood plasma, a straw-colored liquid matrix in which blood cells are suspended. It is an aqueous solution containing about 90% water, 8% soluble blood plasma proteins, 1% electrolytes, and 1% elements in transit. One percent of the plasma is salt, which helps with pH. Human blood plasma volume averages about 2.7–3.0 liters.
Molecular Contents of Plasma

Composition of Blood: Two tubes of EDTA-anticoagulated blood. Left tube: after standing, the RBCs have settled at the bottom of the tube.
Plasma contains molecules that are transported around the body. Respiratory gases, such as oxygen and carbon dioxide, may be dissolved directly in the plasma. However, most oxygen is hemoglobin bound, and most carbon dioxide is converted to bicarbonate ions in the plasma. Hormones and nutrients such as glucose, amino acids and proteins, lipids and fatty acids, and vitamins are also dissolved in the plasma. Waste products are carried through the plasma during their removal, including urea and ammonia.
Plasma Proteins
The largest group of solutes in plasma contains three important proteins: albumins, globulins, and clotting proteins.
Albumins
Albumins, produced in the liver, make up about two-thirds of the proteins in plasma. Albumins maintain the osmotic balance between the blood and tissue fluids. These proteins exert a force that pulls water towards them, which is called oncotic or osmotic pressure. During inflammation, albumins leave the vascular endothelium and enter the tissues, which transports water and some of the plasma into the interstitial fluid. This is the principal cause of exudate edema, which is the swelling that indicates inflammation.
Albumins also assist in transport of different materials, such as vitamins and certain molecules and drugs (e.g. bilirubin, fatty acids, and penicillin) due to the force exerted by their oncotic pressure. Plasma that is pulled into the tissues by albumin-exerted oncotic pressure becomes interstitial fluid. This gradually drains into the lymphatic system which it turn recirculates it back into the plasma of the circulatory system.
Globulins
Globulins are a diverse group of proteins designated into three groups, gamma, alpha, and beta, based on how far they move during electrophoresis tests. Their main function is to transport various substances in the blood. For example, the beta globulin transferrin can transport iron. Most gamma globulins are antibodies (immunoglobulin), which assist the body’s immune system in defense against infections and illness. Alpha globulins are notable for inhibiting certain proteases, while beta globulins often function as enzymes in the body.
Clotting Factors
Clotting proteins are mainly produced in the liver. Twelve proteins known as “clotting factors” participate in the cascade clotting process during endothelial injury. One important clotting factor is fibrinogen. Fibrinogen generates fibrin when activated by the coagulant thrombin, which forms a mesh that clots blood with the assistance of a platelet plug. Normally, anticoagulants and fibrinolytics in the plasma, such as plasmin and heparin, break up fibrin clots and inactivate thrombin. However, during endothelial injury, damaged cells will release tissue factor, another type of clotting factor that causes a cascade of thrombin production that will overpower the anticoagulants and cause a clotting response.
Serum is a term used to describe plasma that has been removed of its clotting factors. Serum still contains albumin and globulins, which are often called serum proteins as a result.

