153 The Large Intestine
Anatomy of the Large Intestine
The large intestine absorbs water from the remaining indigestible food matter and compacts feces prior to defecation.
Learning Objectives
Describe the function and anatomy of the large intestine
Key Takeaways
Key Points
- The large intestine starts in the right iliac region of the pelvis, just at or below the right waist, where it is joined to the bottom end of the small intestine. It is about 4.9 feet (1.5 m) long, which is about one-fifth of the whole length of the intestinal canal.
- The appendix is attached to its inferior surface of the cecum. It contains the least lymphoid tissue, and it is a part of mucosa-associated lymphoid tissue that gives it an important role in immunity.
- On the surface of the large intestine, three bands of longitudinal muscle fibers called taeniae coli, each about 0.2 inches wide, can be identified. They start at the base of the appendix and extend from the cecum to the rectum.
Key Terms
- appendix: An inner organ without any known use that can become inflamed.
- cecum: A pouch, usually peritoneal, that is considered to be the beginning of the large intestine.
- colon: The part of the large intestine that is the final segment of the digestive system, after (distal to) the ileum and before (proximal to) the anus.
Function and Form of the Large Intestine
The function of the large intestine (or large bowel) is to absorb water from the remaining indigestible food matter, and then to pass the useless waste material from the body. The large intestine consists of the cecum and colon.
Large intestine: A schematic of the large intestine, with the colon marked as follows: cecum; 1) ascending colon; 2) transverse colon; 3) descending colon; 4) sigmoid colon, rectum, and anus.
It starts in the right iliac region of the pelvis, just at or below the right waist, where it is joined to the bottom end of the small intestine (cecum). From here it continues up the abdomen (ascending colon), then across the width of the abdominal cavity (transverse colon), and then it turns down (descending colon), continuing to its endpoint at the anus (sigmoid colon to rectum to anus). The large intestine is about 4.9 feet (1.5 m) long—about one-fifth of the whole length of the intestinal canal.
Differences Between Large and Small Intestine
The large intestine differs in physical form from the small intestine in several ways. The large intestine is much wider, and the longitudinal layers of the muscularis are reduced to three, strap-like structures known as the taeniae coli.
The wall of the large intestine is lined with simple columnar epithelium. Instead of having the evaginations of the small intestine (villi), the large intestine has invaginations (the intestinal glands).
While both the small intestine and the large intestine have goblet cells, they are more abundant in the large intestine.
Additional Structures
The appendix is attached to its inferior surface of the cecum. It contains the least lymphoid tissue, and it is a part of mucosa-associated lymphoid tissue, which gives it an important role in immunity.
Appendicitis is the result of a blockage that traps infectious material in the lumen. The appendix can be removed with no apparent damage or consequence to the patient.
On the surface of the large intestine, bands of longitudinal muscle fibers called taeniae coli, each about 0.2 inches wide, can be identified. There are three bands, starting at the base of the appendix and extending from the cecum to the rectum.
Along the sides of the taeniae, tags of peritoneum filled with fat, called epiploic appendages (or appendices epiploicae) are found. The sacculations, called haustra, are characteristic features of the large intestine, and distinguish it from the small intestine.
Histology of the Large Intestine
The large intestine has taeniae coli and invaginations (the intestinal glands), unlike the small intestines.
Learning Objectives
Describe the histology of the large intestine
Key Takeaways
Key Points
- The longitudinal layer of the muscularis of the large intestine is reduced to three, strap-like structures known as the taeniae coli—bands of longitudinal muscle fibers, each about 1/5 in wide.
- The bands of longitudinal muscle fibers start at the base of the appendix and extend from the cecum to the rectum.
- The wall of the large intestine is lined with simple columnar epithelium.
- Both the small intestine and the large intestine have goblet cells, but they are abundant in the large intestine.
Key Terms
- goblet cell:
- columnar epithelium: Epithelial cells whose heights are at least four times their width.
- mucin: A family of high molecular weight, heavily glycosylated proteins (glycoconjugates) produced by the epithelial tissues in most metazoans.
- goblet cells: Glandular, simple, columnar epithelial cells whose sole function is to secrete mucin, which dissolves in water to form mucus.
Histology of the Large Intestine

Colon biopsy: Micrograph of a colon biopsy.
The large intestine, or large bowel, is the last part of the digestive system in vertebrate animals. Its function is to absorb water from the remaining indigestible food matter, and then to pass the useless waste material from the body. The large intestine consists of the cecum, colon, rectum, and anal canal.
It starts in the right iliac region of the pelvis, just at or below the right waist, where it is joined to the bottom end of the small intestine. From here it continues up the abdomen, across the width of the abdominal cavity, and then it turns downward, continuing to its endpoint at the anus.
The large intestine differs in physical form from the small intestine in being much wider. The longitudinal layer of the muscularis is reduced to three strap-like structures known as the taeniae coli—bands of longitudinal muscle fibers, each about 1/5 in wide. These three bands start at the base of the appendix and extend from the cecum to the rectum.
Along the sides of the taeniae are tags of peritoneum filled with fat; these are called epiploic appendages, or appendices epiploicae. The wall of the large intestine is lined with simple columnar epithelium.
Instead of having the evaginations of the small intestine ( villi ), the large intestine has invaginations (the intestinal glands). While both the small intestine and the large intestine have goblet cells that secrete mucin to form mucus in water, they are abundant in the large intestine.

Sigmoid colon: A photograph of the large bowel (sigmoid colon) that shows multiple diverticula on either side of the longitudinal muscle bundle (Taenia coli).
In histology, an intestinal crypt—called the crypt of Lieberkühn—is a gland found in the epithelial lining of the small intestine and colon. The crypts and intestinal villi are covered by epithelium that contains two types of cells: goblet cells that secrete mucus and enterocytes that secrete water and electrolytes.
The enterocytes in the mucosa contain digestive enzymes that digest specific food while they are being absorbed through the epithelium. These enzymes include peptidases, sucrase, maltase, lactase and intestinal lipase. This is in contrast to the stomach, where the chief cells secrete pepsinogen. In the intestine, the digestive enzymes are not secreted by the cells of the intestine.
Also, new epithelium is formed here, which is important because the cells at this site are continuously worn away by the passing food. The basal portion of the crypt, further from the intestinal lumen, contains multipotent stem cells.
During each mitosis, one of the two daughter cells remains in the crypt as a stem cell, while the other differentiates and migrates up the side of the crypt and eventually into the villus. Goblet cells are among the cells produced in this fashion. Many genes have been shown to be important for the differentiation of intestinal stem cells.
The loss of proliferation control in the crypts is thought to lead to colorectal cancer.
Bacterial Flora
The largest bacteria ecosystem in the human body is in the large intestine, where it plays a variety of important roles.
Learning Objectives
Describe other factors about gut/bacterial flora
Key Takeaways
Key Points
- The large intestine absorbs some of the products formed by the bacteria that inhabit this region, such as short-chain fatty acids that are metabolized from undigested polysaccharides (fiber).
- Other bacterial products of undigested polysaccharide fermentation include gas (flatus), which consists primarily of nitrogen and carbon dioxide.
- These bacteria also produce large amounts of vitamins, especially vitamin K and biotin (a B vitamin), for absorption into the blood.
- Factors that disrupt the microorganism population of the large intestine include antibiotics, stress, and parasites.
Key Terms
- passive diffusion: The net movement of material from an area of high concentration to an area of low concentration without any energy input.
- bacterial flora: A community of bacteria that exists on or in the body, and possesses a unique ecological relationship with the host.
- colitis: An inflammation of the colon or the large intestine.
Bacterial Flora
The large intestine houses over 700 species of bacteria that perform a wide variety of functions; it is the largest bacterial ecosystem in the human body. The large intestine absorbs some of the products formed by the bacteria that inhabit this region.
For example, undigested polysaccharides (fiber) are metabolized to short-chain fatty acids by the bacteria in the large intestine, and then are absorbed by passive diffusion. The bicarbonate that the large intestine secretes helps to neutralize the increased acidity that results from the formation of these fatty acids.
Bacteria and Vitamins
Bacterial flora: Escherichia coli is one of the many species of bacteria present in the human gut.
These bacteria also produce large amounts of vitamins, especially vitamin K and biotin (a B vitamin), for absorption into the blood. Although this source of vitamins, in general, provides only a small part of the daily requirement, it makes a significant contribution when dietary vitamin intake is low.
An individual who depends just on the absorption of vitamins formed by bacteria in the large intestine may become vitamin deficient if treated with antibiotics that inhibit other species of bacteria, as well as the disease-causing bacteria.
Other bacterial products include gas (flatus), which is a mixture of nitrogen and carbon dioxide, with small amounts of hydrogen, methane, and hydrogen sulphide. These are produced as a result of the bacterial fermentation of undigested polysaccharides. The normal flora is also essential for the development of certain tissues, including the cecum and lymphatics.
Bacteria and Antibodies
Bacterial flora is also involved in the production of cross-reactive antibodies. These are antibodies produced by the immune system against the normal flora, that are also effective against related pathogens, and prevent infection or invasion.
The most prevalent bacteria are the bacteroides, which have been implicated in the initiation of colitis and colon cancer. Bifidobacteria are also abundant, and are often described as friendly bacteria.
A mucus layer protects the large intestine from attacks from colonic commensal bacteria. Some factors that disrupt the microorganism population of the large intestine include antibiotics, stress, and parasites.
Digestive Processes of the Large Intestine
In the large intestine, a host of microorganisms known as gut flora help digest the remaining food matter and create vitamins.
Learning Objectives
Summarize the digestive processes of the gut flora of the large intestine
Key Takeaways
Key Points
- The large intestine takes about 16 hours to finish the remaining processes of the digestive system.
- The colon absorbs vitamins created by the colonic bacteria. Gut flora consists of microorganisms that live in the digestive tracts of animals; the digestive tract is the largest reservoir of human flora.
- The colon compacts feces and stores fecal matter in the rectum until it can be defecated.
- The gut flora performs many useful functions, such as fermenting unused energy substrates, training the immune system, preventing the growth of pathogenic bacteria, regulating the development of the gut, producing vitamins for the host, and producing hormones to direct the host to store fats.
Key Terms
- saccharolytic: The breakdown of carbohydrates for energy.
- gut flora: The microorganisms that normally live in the digestive tract of animals.
- vitamin: Any of a specific group of organic compounds essential in small quantities for healthy human growth, metabolism, development, and body function that are found in minute amounts in plant and animal foods or sometimes produced synthetically; deficiencies of specific vitamins produce specific disorders.
Overview of the Large Intestine
Digestive processes in large intestine: This image shows the relationship of the colon to the other parts of the digestive system.
The large intestine takes about 16 hours to finish up the remaining processes of the digestive system. Food is no longer broken down at this stage of digestion. The colon absorbs vitamins created by the colonic bacteria—such as vitamin K (especially important as the daily ingestion of vitamin K is not normally enough to maintain adequate blood coagulation), vitamin B12, thiamine, and riboflavin. It also compacts feces, and stores fecal matter in the rectum until it can be defecated.
Gut Flora
Gut flora consists of microorganisms that live in the digestive tracts of animals—the gut is the largest reservoir of human flora. The human body, which consists of about 10 trillion cells, carries about ten times as many microorganisms in the intestines.
The metabolic activities performed by these bacteria resemble those of an organ, leading some to liken gut bacteria to a forgotten organ. It is estimated that these gut flora have around a hundred times as many genes in aggregate as there are in the human genome.
Bacteria make up most of the flora in the colon and up to 60 percent of the dry mass of feces. Somewhere between 300 and 1000 different species live in the gut, with most estimates at about 500. Ninety-nine percent of the bacteria probably come from about 30 or 40 species.
Research suggests that the relationship between gut flora and humans is not merely commensal (a non-harmful coexistence), but rather a mutualistic relationship. Though people can survive without gut flora, the microorganisms perform a host of useful functions, such as:
- Fermenting unused energy substrates.
- Training the immune system.
- Preventing growth of harmful, pathogenic bacteria.
- Regulating the development of the gut.
- Producing vitamins for the host (such as biotin and vitamin K).
- Producing hormones to direct the host to store fats.
Gut Flora and Specialized Digestion
Bacterial flora: Escherichia coli, one of the many species of bacteria present in the human gut.
Without gut flora, the human body would be unable to utilize some of the undigested carbohydrates it consumes. Some types of gut flora have enzymes that human cells lack for breaking down certain polysaccharides. Carbohydrates that need bacterial assistance for digestion include:
- Certain starches.
- Fiber.
- Oligosaccharides and sugars like lactose (in the case of lactose intolerance) and sugar alcohols.
- Mucus produced by the gut.
- Various proteins.
Fermentation
Bacteria turn the carbohydrates they ferment into short-chain fatty acids (SCFAs) by a form of fermentation called saccharolytic fermentation. These SCFAs include acetic acid, propionic acid, and butyric acid.
SCFAs can be used by host cells as a major source of useful energy and nutrients for humans. They also help the body absorb essential dietary minerals such as calcium, magnesium, and iron. Evidence indicates that bacteria enhance the absorption and storage of lipids and produce and aid the absorption of needed vitamins, such as vitamin K.
Absorption and Feces Formation in the Large Intestine
The large intestine absorbs water from the chyme and stores feces until they can be defecated.
Learning Objectives
Describe the process of absorption and feces formation in the large intestine
Key Takeaways
Key Points
- Partially digested food passes from the small intestine to the large intestine or colon.
- Within the colon, digestion is retained long enough to allow fermentation via gut bacteria that break down some of the substances that remain after processing in the small intestine.
- The large intestine houses over 700 species of bacteria that metabolize polysaccharides into short-chain fatty acids that produce large amounts of vitamins —especially vitamin K and biotin—and gas.
- The normal flora of bacteria in the large intestine is essential in the development of certain tissues, including the cecum and lymphatics.
Key Terms
- feces: Digested waste material that is discharged from the bowels; excrement.
- polysaccharide: A polymer made of many saccharide units that are linked by glycosidic bonds.
- anal sphincter: A ring muscle that surrounds the anus (anal orifice).
After the food has been passed through the small intestine, it enters the large intestine. Within the large intestine, digestion is retained long enough to allow fermentation via gut bacteria that break down some of the substances that remain after processing in the small intestine.
Some of the breakdown products are absorbed. In humans, these include most complex saccharides (at most, three disaccharides are digestible by humans).
Intestinal Bacteria
The large intestine houses over 700 species of bacteria that perform a variety of functions. The large intestine absorbs some of the products formed by the bacteria that inhabit this region.
Undigested polysaccharides (fiber) are metabolized into short-chain fatty acids by bacteria in the large intestine and get absorbed by passive diffusion. The bicarbonate that the large intestine secretes helps to neutralize the increased acidity from the formation of fatty acids.
Intestinal bacteria also produce large amounts of vitamins, especially vitamin K and biotin (a B vitamin), which are absorbed into the blood. Although this source of vitamins provides only a small part of the daily requirement, it makes a significant contribution when dietary vitamin intake is low. An individual that depends on absorption of vitamins formed by bacteria in the large intestine may become vitamin-deficient if treated with antibiotics that inhibit other species of bacteria while targeting the disease-causing bacteria.
Other bacterial products include gas (flatus)—a mixture of nitrogen and carbon dioxide, with small amounts of the gases hydrogen, methane, and hydrogen sulphide. The bacterial fermentation of undigested polysaccharides produces these gases.
Intestinal flora are also essential for the development of certain tissues, including the cecum and lymphatics.
Water and Cellulose
The large intestine absorbs water from the chyme and stores feces until it can be defecated. Food products that cannot go through the villi, such as cellulose (dietary fiber), are mixed with other waste products from the body and become hard and concentrated feces.
The feces is stored in the rectum for a certain period and then the stored feces is eliminated from the body due to the contraction and relaxation of the anus. The exit of this waste material is regulated by the anal sphincter.
Defecation Reflex
Defecation is a combination of voluntary and involuntary processes that create enough force to remove waste material from the digestive system.
Learning Objectives
Describe the defecation reflex
Key Takeaways
Key Points
- The rectal ampulla acts as a temporary storage facility for the unneeded digestive material.
- A sufficient increase in fecal material in the rectum causes stretch receptors from the nervous system that are located in the rectal walls to trigger the contraction of rectal muscles, the relaxation of the internal anal sphincter, and an initial contraction of the skeletal muscle of the external sphincter.
- The relaxation of the internal anal sphincter causes a signal to be sent to the brain indicating an urge to defecate.
- If defecation is delayed for a prolonged period, the fecal matter may harden and autolyze, and result in constipation.
- Once the voluntary signal to defecate is sent back from the brain, the ano-rectal angle decreases, becoming almost straight, and the external anal sphincter relaxes. The rectum contracts and shortens in peristaltic waves, forcing fecal material out of the rectum and down through the anal canal.
Key Terms
- defecation: The act or process of voiding feces from the bowels.
- rectum: The terminal part of the large intestine through which feces pass.
- anal canal: The terminal part of the large intestine, situated between the rectum and anus.
- constipation: A state of the bowels in which the evacuations are infrequent and difficult, or the intestines become filled with hardened feces.
- autolyze: To destroy itself; to be destroyed by its own enzymes.
Examples
Constipation is uncomfortable, but it may be a signal that your diet is deficient in fibrous foods (eat more fruits and vegetables) and that you are not drinking enough water, so laxatives are generally not the best way to treat it.
Defecation
For the adult human, the process of defecation is normally a combination of both voluntary and involuntary processes that create enough force to remove waste material from the digestive system.
The rectal ampulla acts as a temporary storage facility for the unneeded material. As additional fecal material enters the rectum, the rectal walls expand. A sufficient increase in fecal material in the rectum causes the stretch receptors from the nervous system, located in the rectal walls, to trigger the contraction of rectal muscles, the relaxation of the internal anal sphincter, and an initial contraction of the skeletal muscle of the external sphincter. The relaxation of the internal anal sphincter causes a signal to be sent to the brain indicating an urge to defecate.
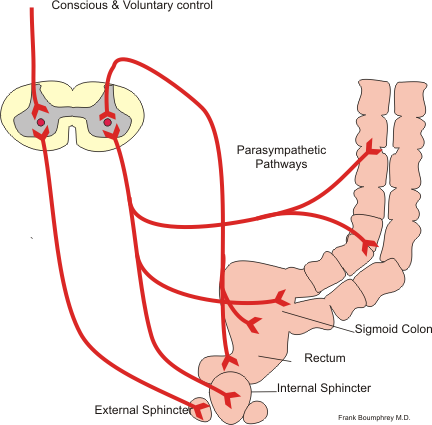
Defecation reflex: The conscious and parasympathetic pathways of the defecation reflex.
If this urge is not acted upon, the material in the rectum is often returned to the colon by reverse peristalsis where more water is absorbed, thus temporarily reducing pressure and stretching within the rectum. The additional fecal material is stored in the colon until the next mass peristaltic movement of the transverse and descending colon. If defecation is delayed for a prolonged period, the fecal matter may harden and autolyze, resulting in constipation.
Once the voluntary signal to defecate is sent back from the brain, the final phase begins. The abdominal muscles contract (straining), causing the intra-abdominal pressure to increase. The perineal wall is lowered and causes the anorectal angle to decrease from 90 degrees to less than 15 degrees (almost straight), and the external anal sphincter relaxes.
The rectum now contracts and shortens in peristaltic waves, thus forcing fecal material out of the rectum and down through the anal canal. The internal and external anal sphincters, along with the puborectalis muscle, allow the feces to be passed by pulling the anus up and over the exiting feces in shortening and contracting actions.



