13 2.5 Head-to-Toe Assessment
Glynda Rees Doyle and Jodie Anita McCutcheon
A comprehensive head-to-toe assessment is done on patient admission, at the beginning of each shift, and when it is determined to be necessary by the patient’s hemodynamic status and the context. The head-to-toe assessment includes all the body systems, and the findings will inform the health care professional on the patient’s overall condition. Any unusual findings should be followed up with a focused assessment specific to the affected body system.
A physical examination involves collecting objective data using the techniques of inspection, palpation, percussion, and auscultation as appropriate (Wilson & Giddens, 2013). Checklist 17 outlines the steps to take.
Disclaimer: Always review and follow your hospital policy regarding this specific skill. |
|
Safety considerations:
|
|
Steps |
Additional Information |
1. General appearance:
|
Alterations may reflect neurologic impairment, oral injury or impairment, improperly fitting dentures, differences in dialect or language, or potential mental illness. Unusual findings should be followed up with a focused neurological system assessment.
 |
| This is not a specific step. Evaluating the skin, hair, and nails is an ongoing element of a full body assessment as you work through steps 3-9.
2. Skin, hair, and nails:
|
Check for and follow up on the presence of lesions, bruising, and rashes.Variations in skin temperature, texture, and perspiration or dehydration may indicate underlying conditions.
Redness of the skin at pressure areas such as heels, elbows, buttocks, and hips indicates the need to reassess patient’s need for position changes. Unilateral edema may indicate a local or peripheral cause, whereas bilateral-pitting edema usually indicates cardiac or kidney failure. Check hair for the presence of lice and/or nits (eggs), which are oval in shape and adhere to the hair shaft. |
3. Head and neck:
|
Check eyes for drainage, pupil size, and reaction to light. Drainage may indicate infection, allergy, or injury.
Slow pupillary reaction to light or unequal reactions bilaterally may indicate neurological impairment.  Dry mucous membranes indicate decreased hydration. Facial asymmetry may indicate neurological impairment or injury. Unusual findings should be followed up with a focused neurological system assessment. |
4. Chest:
|
Chest expansion may be asymmetrical with conditions such as atelectasis, pneumonia, fractured ribs, or pneumothorax.
Use of accessory muscles may indicate acute airway obstruction or massive atelectasis. Jugular distension of more than 3 cm above the sternal angle while the patient is at 45º may indicate cardiac failure. The presence of crackles or wheezing must be further assessed, documented, and reported. Unusual findings should be followed up with a focused respiratory assessment. 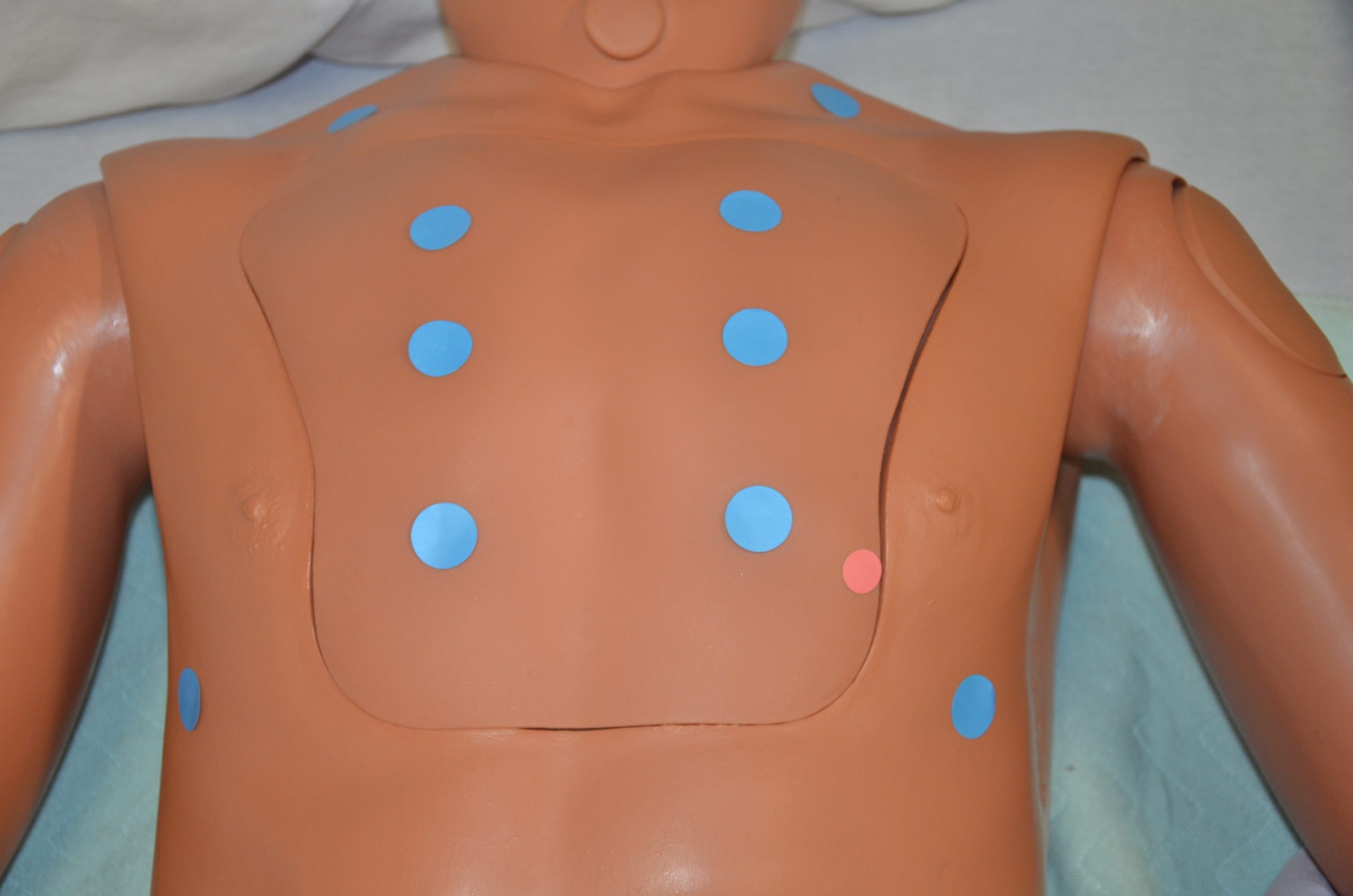  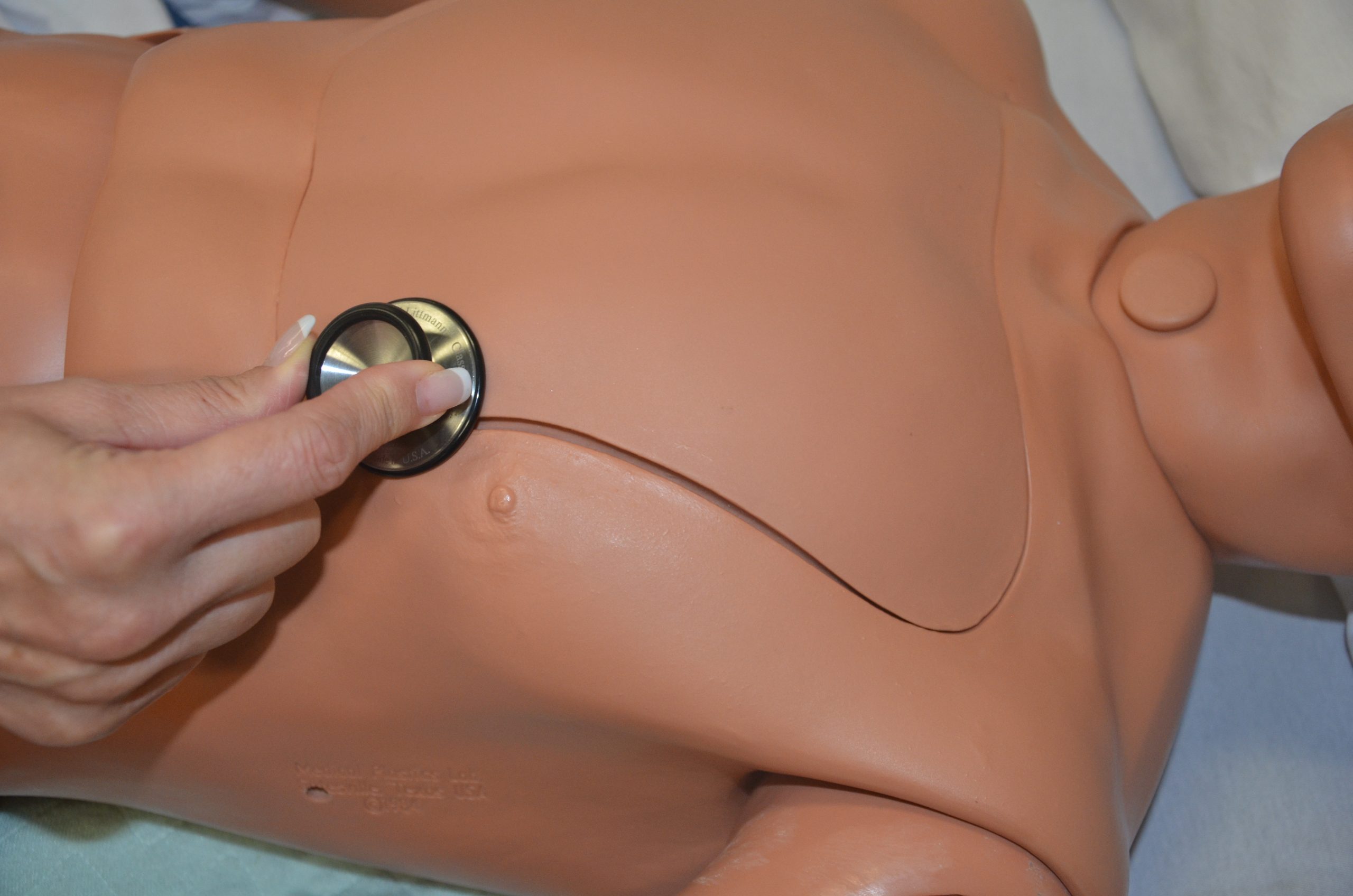 Note the heart rate and rhythm, identify S1 and S2, and follow up on any unusual findings with a focused cardiovascular assessment. |
5. Abdomen:
|
Abdominal distension may indicate ascites associated with conditions such as heart failure, cirrhosis, and pancreatitis. Markedly visible peristalsis with abdominal distension may indicate intestinal obstruction.
Hyperactive bowel sounds may indicate bowel obstruction, gastroenteritis, or subsiding paralytic ileum. Hypoactive or absent bowel sounds may be present after abdominal surgery, or with peritonitis or paralytic ileus. Pain and tenderness may indicate underlying inflammatory conditions such as peritonitis. Unusual findings in urine output may indicate compromised urinary function. Follow up with a focused gastrointestinal and genitourinary assessment. Unusual findings with bowel movements should be followed up with a focused gastrointestinal and genitourinary assessment.  |
6. Extremities:
|
Limitation in range of movement may indicate articular disease or injury.
Palpate pulses for symmetry in rate and rhythm. Asymmetry may indicate cardiovascular conditions or post-surgical complications. Unequal handgrip and/or foot strength may indicate underlying conditions, injury, or post-surgical complications. CWMS: colour, warmth, movement, and sensation of the hands and feet should be checked and compared to determine adequacy of perfusion. Check skin integrity and pressure areas, and ensure follow-up and in-depth assessment of patient mobility and need for regular changes in position.     Palpate and inspect capillary refill and report if more than 3 seconds.   To check capillary refill, depress the nail edge to cause blanching and then release. Colour should return to the nail instantly or in less than 3 seconds. If it takes longer, this suggests decreased peripheral perfusion and may indicate cardiovascular or respiratory dysfunction. Unusual findings should be followed up with a focused cardiovascular assessment. Clubbing of nails, in which the nails present as straightened out to 180 degrees, with the nail base feeling spongy, occurs with heart disease, emphysema, and chronic bronchitis. |
7. Back area (turn patient to side or ask to sit up or lean forward):
|
Check for curvature or abnormalities in the spine.
Check skin integrity and pressure areas, and ensure follow-up and in-depth assessment of patient mobility and need for regular changes in position. |
8. Tubes, drains, dressings, and IVs:
|
Note amount, colour, and consistency of drainage (e.g., Foley catheter), or if infusing as prescribed (e.g., intravenous).
 Assess wounds for large amounts of drainage or for purulent drainage, and provide wound care as indicated. |
9. Mobility:
|
Assess patient’s risk for falls. Document and follow up any indication of falls risk. Note use of mobility aids and ensure they are available to the patient on ambulation.
 |
| 10. Report and document assessment findings and related health problems according to agency policy. | Accurate and timely documentation and reporting promote patient safety. |
| Data source: Assessment Skill Checklists, 2014; Jarvis et al., 2014; Stephen et al., 2012 | |
Critical Thinking Exercises
- You are assessing a patient at the beginning of your shift. Which assessment would be the most appropriate?
- You come back from a break to find your patient complaining that she feels short of breath. Which assessment would be the most appropriate?
Media Attributions
- Book pictures 2015 599

